Von Willebrand’s disease
Von Willebrand’s disease
Updated: 07/25/2023
© Jun Wang, MD, PhD
General features
- Most common hereditary bleeding disorder
- No gender preference, but females tend to be symptomatic with the same von Willebrand Factor (vWF) level
- Due to deficiency or dysfunction of vWF, which has two functions:
Mediating platelet adherence to subendothelium
Carrier molecule for Factor VIII, which protects
it from premature destruction
- Bleeding exacerbated by aspirin
Phenotypes
- Type 1, partial quantitative deficiency of vWF but normal function
Most common, autosomal dominant
- Type 2, qualitative defects
4 subtypes*: A, B, M, N
Autosomal dominant (B), recessive (N), or either
(A, M)
Most common subtype: 2A
- Type 3, severe or complete vWF deficiency
Very rare
Autosomal recessive
Clinical presentations
- Similar to platelet dysfunction: nose bleeding, easy bruising, etc
- Type 1
Mild/moderate bleeding
- Type 2
2A: Moderate to severe bleeding
2B: Moderate to severe bleeding
2M: Moderate to severe bleeding
2N: Joint, soft tissue, urinary bleeding,
similar to hemophilia A
- Type 3
Severe bleeding
Joint and soft tissue bleeding
Key pathogenesis
- Qualitative or quantitative defects of vWF
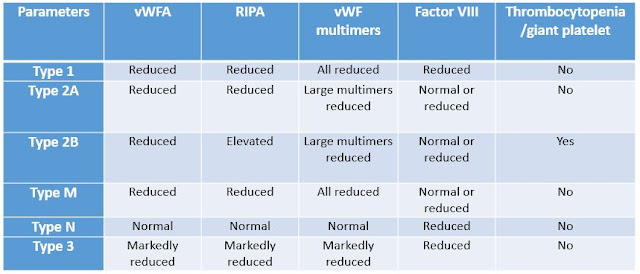
Key Laboratory findings
- Normal or prolonged aPTT
- Normal PT
- Others
vWFA:
von Willebrand factor activity
RIPA:
Ristocetin-induced platelet aggregation
Treatment
- Desmopressin (DDAVP), NOT for type 3
- Recombinant von Willebrand factor (rVWF)
- von Willebrand factor/factor VIII (vWF/FVIII) concentrates
- Antifibrinolytic drugs
- Platelet transfusion
* A subtype, 2C, was proposed in
2009
Back to bleeding disorders
Back to contents
Comments
Post a Comment