Osteosarcoma
Osteosarcoma
Updated: 09/24/2018
© Jun Wang,
MD, PhD
General features
- Any malignant tumors that produce osteoid directly from tumor cells
- Most common primary bone tumor after myeloma
- Young age, 10-25
- Most common metastasis site: Lung
- Rare metastasis to lymph nodes
Risk factors
If > 40
- Paget disease
- Radiation exposure
- Thorotrast
- Childhood chemotherapy
- Other bone disorders such as fibrous dysplasia, osteochondromatosis, chondromatosis, etc
Clinical presentations
- Most common clinical presentation: Localized pain
- Mass
Most common site
- Metaphysis of long bones, especially around the knee
- Medullary cavity
Key pathogenesis
- Unclear, probably associated with rapid bone growth
Key laboratory findings
- Elevated alkaline phosphatase
Key radiological findings
- Large, destructive mass
- Lytic or blastic
- Permeative margins
- Sunburst pattern due to bone formation
- Codman’s triangle: Shadow between cortex and raised ends of periosteum (due to reactive bone formation), non-specific (can be seen in Ewing sarcoma)
Key morphological features
- Most commonly metaphysis
- Bulky invasive mass with hemorrhage and necrosis
- Pleomorphic tumor cells with osteoid matrix
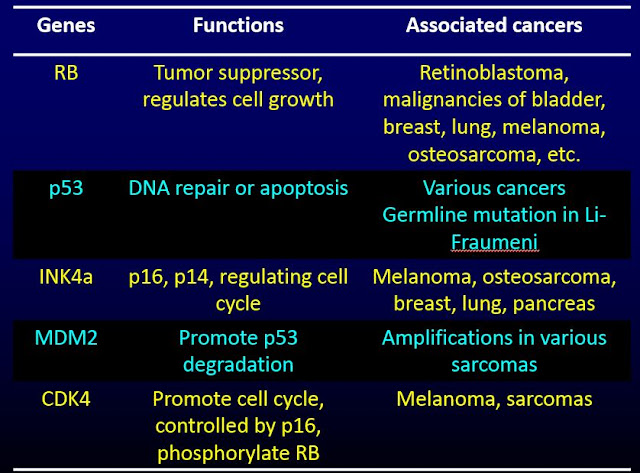
Genetic abnormalities
- Combined p53 and Rb mutation common
- P53 mutations if multicentric
Negative prognosis indicator
- Paget disease
- Telangiectatic histology
- Elevated serum alkaline phosphatase
- Minimal postchemotherapy tumor necrosis
- Involvement of craniofacial bones (not jaw) or vertebrae
- Multifocal tumor
- Loss of heterozygosity of RB gene
Treatment
- Surgery
- Chemotherapy
Back to contents
Comments
Post a Comment