Pulmonary hypertension due to lung disease and or hypoxia
Pulmonary hypertension due to lung disease and or hypoxia
Updated: 10/12/2022
© Jun Wang, MD, PhD
General features
- Group 3 pulmonary hypertension
- Caused by chronic lung diseases or conditions resulting hypoxemia
- More common in elder population
- Usually associated with increased morbidity and mortality
- Associated disorders include
- Obstructive lung disease (COPD or bronchiectasis)
- Restrictive lung disease (eg, interstitial lung disease, kyphoscoliosis)
- Lung disease with mixed obstruction and restriction (eg, pulmonary fibrosis with emphysema)
- Hypoxia without lung disease (eg, high altitude, sleep-disordered breathing, obesity hypoventilation)
- Developmental lung disorders (eg, bronchopulmonary dysplasia, congenital lobar emphysema)
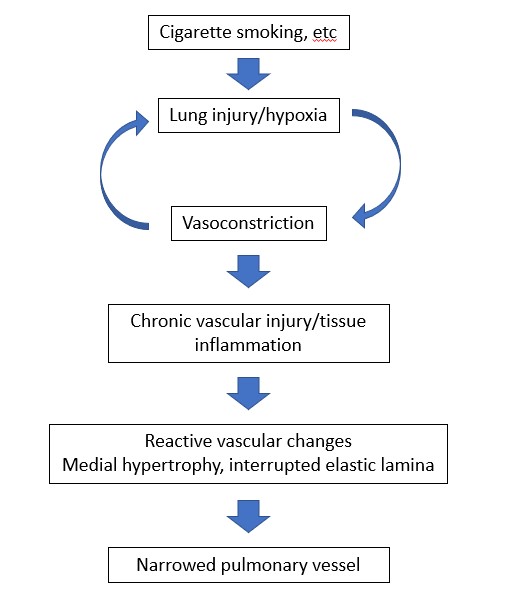
Pathogenesis
- Pulmonary inflammation/hypoxia result in pulmonary vasoconstriction and remodeling
Clinical presentations
- Presentations of underlying lung diseases
- History
- Exertional hyspnea or hypoxemia unexplainable by current lung disorders
- Rapid decline of arterial oxygenation
- Presentations of right heart failure
- PE
- Increased P2 heart sound
- Systolic ejection murmur
- Signs of right sided heart failure: right ventricular heave, elevated jugular vein, hepatomegaly, etc
Key morphological features
- Similar to pulmonary arterial hypertension (PAH)
- Proliferative vasculopathy
- Involving small muscular arteries
- Hyperplasia/hypertrophy of all three layers of vascular wall (intima, media, adventitia)
- Fibrosis
- Thrombi
Diagnosis
- Confirmation of pulmonary hypertension
- Chest X-ray
- Enlarged central pulmonary arteries and peripheral attenuation
- Right heart dilation
- Doppler echocardiography
- Most reliable non-invasive method
- Estimate pulmonary artery pressure
- Tricuspid regurgitation
- Ventilation-perfusion lung scanning: rule out embolism
- Right-sided cardiac catheterization
- Pulmonary function tests, etc
Treatment
- Management of underlying lung diseases
- Supportive approaches: Vaccinations, oxygen, diuretics, smoking cessation, etc
Back to pulmonary hypertension
Back to contents
Comments
Post a Comment