Escherichia coli
Escherichia coli
Updated: 01/30/2024
© Jun Wang, MD, PhD
General features
- Anaerobic G- bacteria, part of normal intestinal flora
- Most common cause of bacterial diarrhea worldwide
- Infections due to disruption of the mucosa
- Most ferment sorbitol (dark pink colonies), except EHEC O157:H7 (white colonies), on MacConkey agar
- 5 commonly seen diarrhea-associated groups
- ETEC: Enterotoxigenic E coli, watery diarrhea
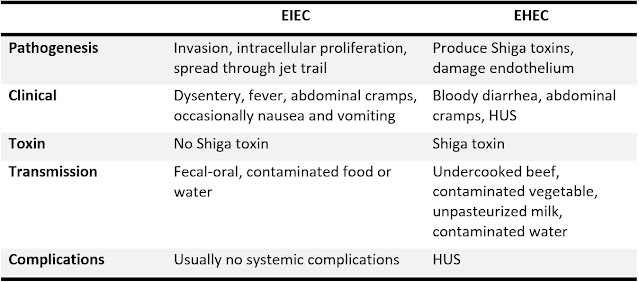
- EIEC: Enteroinvasive E coli, dysentery
- EHEC: Enterohemorrhagic E coli, hemorrhagic colitis and hemolytic uremic syndrome
- EPEC: Enteropathogenic E coli, infantile diarrhea
- EAEC: Enteroaggregative E coli, persistent diarrhea in children and patients infected with HIV
Enterotoxigenic E. coli
- Major cause of “traveler’s diarrhea” and diarrhea in <3-year-olds in developing countries
- Bind to small intestine epithelium through colonization factors (CFs)
- Capsule resistant to phagocytosis
- Two enterotoxins, detectable by immunoassay, etc
- LT: heat-labile, activates adenylate cyclase, ↑cAMP, watery diarrhea due to outflow of chloride and water in small intestine
- ST: heat-stable, diarrhea by stimulating guanylate cyclase
- Usually 4-14 days after infection
- Nausea, watery diarrhea, but usually NO vomiting
- Diagnosis: molecular detection of the genes for LT or ST
Enteroinvasive E. coli
- Large bowel invasion, similar to shigellosis, including the formation of actin “jet trails”
- May have fever >101°F and tenesmus
- Watery diarrhea and excess of leukocytes
- Approximately 10% cases develop dysentery
Enterohemorrhagic E. coli
- AKA verotoxin-producing E. coli (VTEC)
- Most common serotype: O157:H7
- Transmitted through products contaminated with bovine feces
- Non-invasive, NO persistent fever
- Presentations vary, mild diarrhea to hemorrhagic colitis
- May cause hemolytic uremic syndrome (HUS)
Diagnostic approaches
- Culture: Colorless (white) colonies on sorbitol MacConkey
- Shiga toxin enzyme immunoassay following culture
- Molecular testing: Shiga-toxin genes
Managements
- Reduce risk of HUS
- Management of fluid loss, pain (NO opioid), HUS, etc
- Antibiotics NOT recommended: Not needed, or may increase toxin release
- Antibiotics for severe cases NOT associated with Shiga-toxin producing e coli
Back to Infectious gastroenteritis
Back to Contents
Comments
Post a Comment