Infectious gastroenteritis
Infectious gastroenteritis
Updated: 01/26/2024
© Jun Wang, MD, PhD
General features
- Inflammation of GI tract
- Most commonly caused by viruses
- May be associated with bacteria, fungi or parasites
- Fecal-oral transmission: foodborne, waterborne
- Most important risk factor: poor hygiene and sanitation
- Presentations: abdominal pain, nausea/vomiting, diarrhea
- Mild cases
- Most common
- Likely self-limited
- Supportive therapy only
- Severe cases
- May cause dehydration and sepsis
Diarrhea vs. Dysentery
- Diarrhea
o Passage of loose or watery stools
o At least 3 times in a 24-hour period
o Increased water content due to impaired water absorption or active water secretion, with or without mucosa injury or inflammation
o Acute: < 14 days; Persistent: 14-30 days; Chronic: > 30 days
- Dysentery
o AKA invasive diarrhea
o Diarrhea with visible blood or mucus
o Commonly associated with fever and abdominal pain
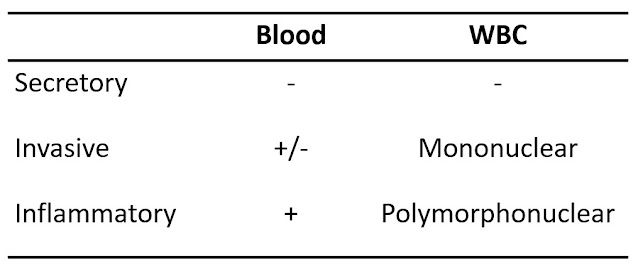
Types of diarrhea
- Secretory
o Due to excessive secretion and/or impaired absorption
o Results in increased fluid and electrolytes in GI tract
- Invasive
o Pathogen penetrates epithelium
o Symptoms associated with enterotoxins, prostaglandins, and impaired reabsorption of fluids and electrolytes
o With visible blood or mucus
- Inflammatory
o Functional disruption due to mucosa inflammation
o Cause by cytotoxin from non-invasive pathogens
Pathophysiology
- Adherence
- Mucosal invasion
- Enterotoxin production
o Enterotoxigenic E. coli, Vibrio Cholera, etc
o Active secretion results in copious watery diarrhea
- Cytotoxin production
o Shigella dysenteriae, Clostridium difficile, enterohemorrhagic E coli, etc
o Mucosal injury causes blood and inflammatory cells in stool
o Decrease absorptive ability
Diagnostic approaches
- Most cases are mild and self-limited and need no clinical evaluation
- Evaluations needed if persistent fever, bloody diarrhea, abdominal pain, signs of dehydration (oliguria, dark urine)
- History: Especially food taken, residence, recent travel, antibiotic treatment, etc
- PE: evaluate volume status and identify complications
- Lab tests
- CBC, metabolic panel, renal function, etc
- Stool: Pathogen identification (culture, molecular panels, Shiga toxin, C. difficile, entamoeba, etc)
- Specimens that test positive for a bacterial pathogen on a molecular panel (or other culture-independent test) should be submitted for confirmatory culture
Commonly seen food-borne pathogens
Viral gastroenteritis
Parasitic gastroenteritis
Back to contents

Comments
Post a Comment