Nephronophthisis
Nephronophthisis
Updated: 09/30/2021
© Jun Wang, MD, PhD
General features
- Heterogeneous group
- Autosomal recessive
- Most common genetic cause of pediatric end stage kidney disease
- Characterized by corticomedullary cysts, atrophy and interstitial fibrosis
- Diagnosis based on clinical findings and confirmed by genetic testing
Key pathogenesis
- Cilia/basal body abnormality
- Abnormal renal tubular development and function
Clinical presentations
- Infantile
Most severe form
Bilateral disease
Median age for renal failure: 1 year of age
Extrarenal presentations common: retinitis
pigmentosa, hepatic fibrosis, skeletal / CNS malformations, situs inversus, etc
- Juvenile form
Most common
Polyuria/polydipsia
due to cortical and tubulointerstitial damage
Progresses to
chronic renal failure in 5-10 years
Anemia and growth
retardation
May be associated with retinitis pigmentosa
- Adolescent form: Similar to juvenile with later
presentation (median age renal failure, 19 years)
- Extraneral manifestations
Bone: Mainzer-Saldino
syndrome (cone-shaped epiphyses, retinal degeneration and cerebellar
ataxia); RHYNS syndrome (retinitis
pigmentosa, hypopituitarism, NPHP, skeletal dysplasia), etc
Liver:
Hepatosplenomegaly and portal fibrosis with NO or only mild bile
duct proliferation
Situs inversus: Arrangement of the internal
organs as mirror image of normal anatomy; infantile NPHP and mutation in the
NPHP2 gene
Septal cardiac defects if NPHP2 and NPHP3
mutations
Pathological findings
- Normal or small sized kidneys
- Cysts at corticomedullary junction
- Severe tubular atrophy with thick basement membranes, interstitial fibrosis and chronic inflammation
Genetic abnormalities
- Mutation of NPHP1 (Nephronophthisis 1): Encode nephrocystin-1
- Mutation of NPHP2 (inversin) mutation
- Others
Features suggestive of NPHP
- Infantile or young child (<5): End-stage renal disease (ESRD), severe hypertension, and extrarenal anomalies
- Older children and adolescents
- Polyuria and polydipsia
- Progressive chronic kidney disease (CKD) with normal blood pressure
- Absence of proteinuria or mild tubular proteinuria
- Absence of hematuria and cellular elements
- Normal or slightly decreased-in-size kidneys with increased echogenicity, reduced corticomedullary differentiation, and renal cysts on ultrasound examination
- Clinical: Child with renal and extrarenal manifestations, including retina, ocular movement abnormalities, cardiac malformations, etc
- Radiologic studies: Small kidneys with poor corticomedullary differentiation
- Genetic testing: NPHP mutation
- Renal biopsy if genetic testing negative or unavailable
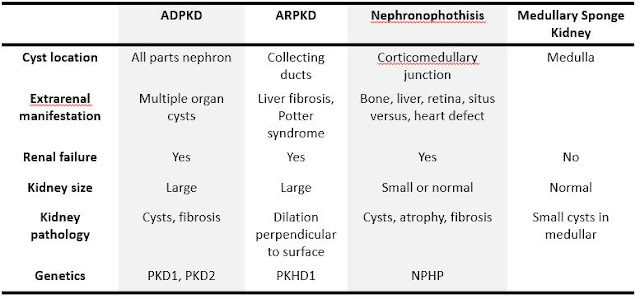
Differential diagnosis
- Autosomal dominant polycystic kidney disease: Cystic changes involving other organs, but congenital liver fibrosis, PKD1 or PKD2 mutation
- Autosomal recessive polycystic kidney disease: Cystic changes in both cortex and medulla, dilatation perpendicular to renal surface, congenital liver fibrosis, Potter syndrome, PKHD1 mutation
- Glomerulocystic cortical cysts: Associated with tuberous sclerosis, trisomy 13 etc
- Medullary cystic kidney disease: Cysts in medulla, NO extrarenal involvement, adult-onset renal failure
- Correction of water and electrolyte imbalances
- Renal transplantation
- Erythropoietin and iron if anemic
- Vitamin D and phosphate binder if secondary hyperparathyroidism
Back to kidney
masses
Back to contents
Comments
Post a Comment