Pathology of parathyroid
Pathology of parathyroid
Updated: 07/02/2023
© Jun Wang, MD, PhD
Anatomy/histology
- Usually four glands between thyroid glands and trachea
- Encapsulated glands with two types of cells
Chief cells:
Small round nuclei, produce parathyroid hormone
Oxyphil cells:
Eosinophilic granular cytoplasm, unknown function
- May contain scattered adipocytes
Parathyroid
hormone
- Secreted in response to low blood calcium
- Maintain calcium homeostasis with calcitonin, produced by C cell of thyroid
- Binding to its receptor stimulates cAMP and phosphatidylinositol diphosphate
- Five major functions:
Activates and
increases the number of osteoclasts
Increases
renal tubular reabsorption of calcium
Increases
conversion of Vitamin D to active
dihydroxy form in kidneys
Increases
urinary phosphate excretion to reduce
calcium loss
Increases GI calcium absorption
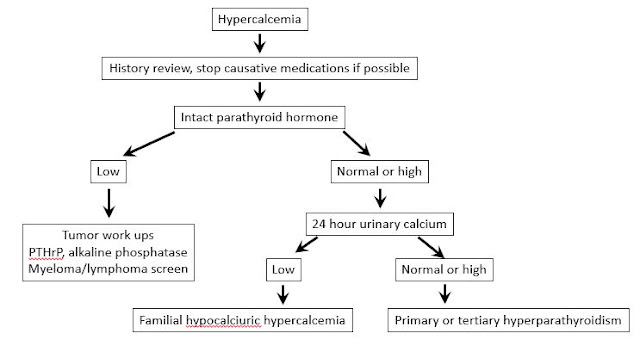
Diagnostic approaches
- Laboratory studies: calcium, intact parathyroid hormone, parathyroid hormone related peptide (if high calcium, low PTH, likely tumor associated), renal function, etc
- Image studies:
- Identify enlarged parathyroid gland/glands, sonography preferred
- Sestamibi: Adenoma vs hyperplasia
- CT, MRI, etc
Hyperparathyroidism
Lack obvious
signs and symptoms associated to excess calcium or parathyroid hormone
Usually
incidental findings of elevated PTH with or without hypercalcemia
May progress
to symptomatic hyperparathyroidism
Hypercalcemia
without elevated PTH is most commonly caused by malignancy
Neoplasm
of parathyroid gland
Back to pathology
of endocrine system
Back to contents
Comments
Post a Comment