Chronic pancreatitis
Chronic pancreatitis
Updated: 03/25/2019
© Jun Wang,
MD, PhD
General features
- Continuing, chronic, inflammatory process
- Irreversible loss of pancreatic parenchyma and replacement with fibrosis
- Variable pancreatic insufficiency (malabsorption, diabetes)
- More common in men, 40+ years of age, alcoholics
- May simulate or coexist with pancreatic carcinoma
- Complications: Pseudocysts; widespread fat necrosis (from liberation of lipase), localized portal hypertension due to fibrosis of splenic vein in alcoholic hepatitis
Etiology
- Commonly idiopathic
- Alcohol: most common etiology (60-70%)
- Intraductal plugging and obstruction: Stones, tumors
- Toxins and toxic metabolites: Promotes release of cytokines
- Oxidative stress: Idiopathic pancreatitis
- Necrosis-fibrosis: Recurrent acute pancreatitis that heals with fibrosis
- Ischemia: From obstruction and fibrosis; important in exacerbating disease
Pathogenesis
- Destruction of pancreatic tissue due to recurrent inflammation
- Fibrosis induced by TGF-beta, PDGF, etc
Clinical presentations
- Precipitated by alcohol, overeating, opiates, other drugs
- Clinical triad of steatorrhea, diabetes and pancreatic calcification
Key pathological features
- Diffuse fibrosis
- Loss of acini and ductal tissue
- Relatively normal islets at early stage
- Intraductal calculi may present
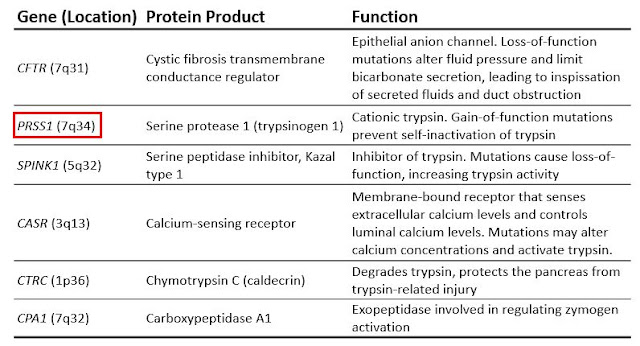
Hereditary pancreatitis
- Recurrent severe acute pancreatitis
- Beginning in childhood and ultimately leading to chronic pancreatitis
- Abnormally increases or sustains the activity of trypsin
- Most common: Gain-of-function mutations of trypsinogen (PRSS1)
- Higher risk of pancreatic cancer
Treatment
- Pancreatic duct drainage, Whipple resection (relieves pain in 50% of patients with pain)
Back to exocrine pancreas pathology
Back to contents
Comments
Post a Comment