Pancreatic cancer
Pancreatic cancer
Updated: 02/04/2025
© Jun Wang, MD, PhD
General features
- Classification based on differentiation: ductal, endocrine, acinar, etc
- Majority are ductal carcinoma
- Fourth leading cause of death
- More common in population older than 50
- 3 recognized precursors of invasive disease: PanIN, IPMN and mucinous cystic neoplasm
- Most common in head and body
- Overall poor prognosis
Clinical presentations
- Non specific: Anorexia, malaise, nausea, fatigue, and midepigastric or back pain
- Painless obstructive jaundice: Most characteristic sign of cancer of head of the pancreas
Risk factors
- Smoking, obesity, diabetes mellitus, chronic pancreatitis
- Genetic abnormalities
Molecular abnormality
- KRAS, SMAD4, CDKN2A, p53, BRCA2, etc
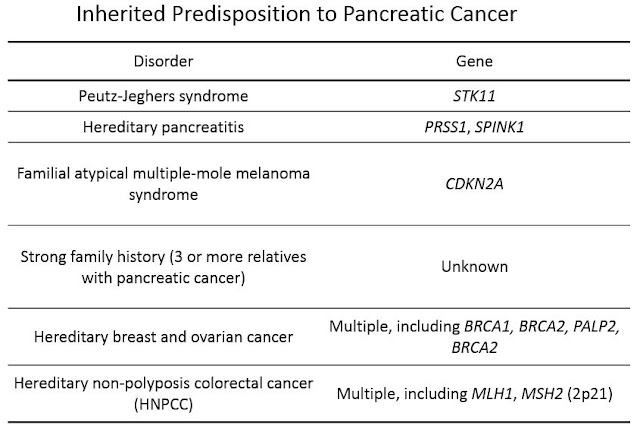
- Inherited
Ductal adenocarcinoma
- Most common pancreatic cancer
- Non specific presentation including pain, weight loss, anorexia, malaise, weakness
- Trousseau sign: Migratory thrombophlebitis, due to tumor or tumor necrosis producing platelet-aggregating factors and procoagulants; causes arterial and venous thrombi, including pulmonary thromboemboli
- Poorly circumscribed, gritty, gray-white, hard masses
- Malignant tubular glands infiltrating desmoplastic stroma
- Loss of nuclear SMAD4 expression
- Serum tests: CEA, CA19-9
Acinar cell carcinoma
- Morphological resemblance to acinar cells
- Produce pancreatic exocrine enzymes (trypsin, chymotrypsin, lipase, etc)
- Resembles similar tumor in salivary gland morphologically
- 1-2% of pancreatic malignancies
- More common in men
- May present with lipase hypersecretion syndrome (subcutaneous fat necrosis)
- Well circumscribed, soft/fleshy with fibrous septa
- Highly cellular with minimal stroma and no desmoplasia
Pancreatoblastoma
- Rare
- More common in children
- Squamous islands admixed with acinar cells
- Poor prognosis if in adults
Pancreatic intraepithelial neoplasia
- PanIN
- Most common precursor lesions of pancreatic ductal adenocarcinoma
- Usually < 5 mm and confined to pancreatic ducts
- Low or high grade, based on epithelial dysplasia
- Papillary or flat, noninvasive epithelial neoplasms
- Composed of columnar to cuboidal cells with variable mucin
Management
- Surgery: Whipple procedure
- Chemotherapy, radiation therapy
Back to contents
Comments
Post a Comment