Practice questions answers coagulopathy
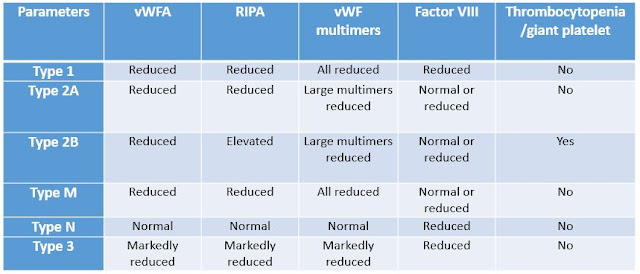
Practice questions answers Coagulopathy © Jun Wang, MD, PhD 1. E. Bleeding disorders with normal platelet counts are commonly associated with coagulation factor abnormalities, either due to factor deficiency or presence of inhibitors. Correction of PT or PTT by mixing studies rules out presence of inhibitors, usually antibodies against coagulation factors. Liver disease associated coagulopathy usually have prolonged PT and PTT. Renal function abnormality can be seen in thrombotic thrombocytopenic purpura or hemolytic-uremic syndrome and atypical hemolytic-uremic syndrome . Vitamin B12 and folate deficiencies are associated with megaloblastic anemia. These are less likely due to normal CBC. 2. B. Factor VIII is low in patients with von Willebrand disease , since von Willebrand factors are carriers of factor VIII. Lacking of von Willebrand factors will influence stabilization of factor VIII. This is less likely to be either Hemophilia A or Hemophilia B since the later tw